Date
Key Points
- Recent studies show that physical activity strengthens your immune system
- Physical Therapist are experts in human movement
- Physical Therapist can help you with more that just your injuries
Physical Therapy Isn’t Just For Pain. It Can Keep You Healthy For Life.
You know that physical activity is good for you. The benefits are well researched and the list is
impressive. Here’s just a sampling:
● Releases endorphins to make you feel good and fight depression
● Helps control weight
● Prevents diseases like stroke, diabetes and some forms of cancer
● Improves sleep
● Helps you live longer
Recent studies even show that physical activity strengthens your immune system, with a
protective effect against COVID, and that staying active through middle age protects your brain
as you age.
Physical activity is a wonder drug. If it was a pill, you’d buy it and take it every day. But even
though activity is free, less than 25% of Americans meet the CDC recommendations for activity.
We clearly need help.
Physical Therapists Are The Experts in Human Movement
To be active, you need to be able to move. Physical Therapists do more than help you recover
from surgeries or major injuries. They are the experts in human movement. Sure, you could see
a strength coach to lift weights, hire a personal trainer, go to a yoga class to work on your
flexibility and balance, and see a chiropractor for adjustments. But that seems like a lot of
people when a PT can help you with all of these things and more. Nobody knows more about
human movement or looks at your health the same way a PT does. Your PT can help you
with every aspect of movement including strength, range of motion, flexibility, endurance,
balance and coordination.
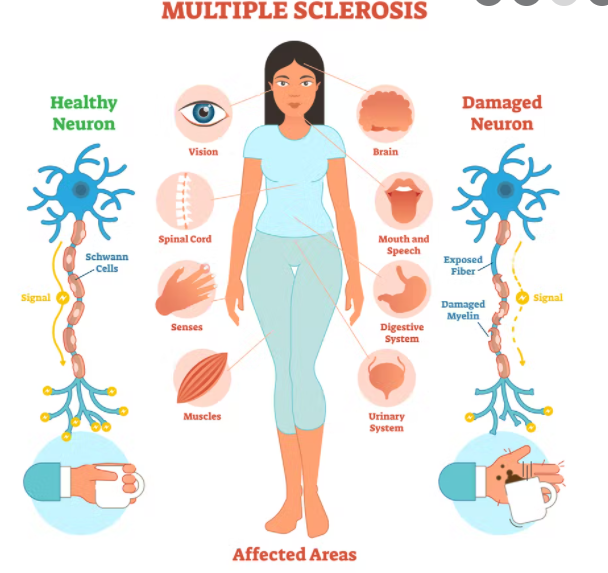
As medical professionals they can help you with injuries or other issues. Your PT can work with
your doctor to help use activity to manage things like diabetes, cholesterol levels or blood
pressure instead of prescriptions. Your PT is also trained to work with people of all ages, so you
can develop a long-term relationship and they can continue to adjust and modify your routine as
you age or your goals change.